Education + Tailored Advice = Informed Decision Making & Better Health Outcomes
Treatment options for managing obesity and metabolic health complications
Some of the non-surgical methods include:
(1) Lifestyle modification alone: FOUNDATION upon which other adjunct therapies will be built upon. It's also the critical component for chronic disease management to promote well-being and the best possible quality of life.
- Healthy eating habits: The goal is to get the correct nutrients that your body needs, by eating healthy foods such as lean meat, fish, nuts, whole grains, vegetables, and fresh fruits. Whereas foods rich in saturated and trans-fat, such as sausages, processed meat, added sugars, baked and fried food should be avoided. Also, cutting back on the quantity of food intake by serving less food on smaller plates, will help you limit your calorie intake.
- Physical activity: Exercise can be broken into structured exercise at the gym/ exercise class etc and incidental physical activity. The benefits of exercise are many and include:
- reducing the risk of heart disease, type 2 diabetes, and some cancers,
- helps to strengthen your muscles, bones and joints,
- and improves the working of your heart and lungs.
- reduces your stress levels, and may also improve your mental health and wellbeing.
Individuals with musculoskeletal ailments or limited mobility may need alternative forms of exercise such as water-based activities. Furthermore, individuals with cardiovascular or respiratory disease may also need a gentler exercise regime prescribed by an exercise physiologist. If you are unsure, please ask your regular GP or Dr Rigas during your consultation.
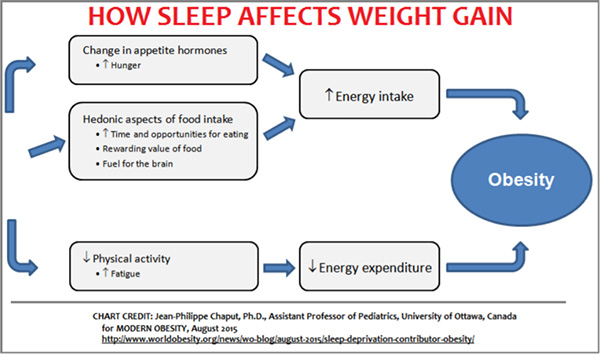
(2)Sleep Hygiene: Improve sleep hygiene
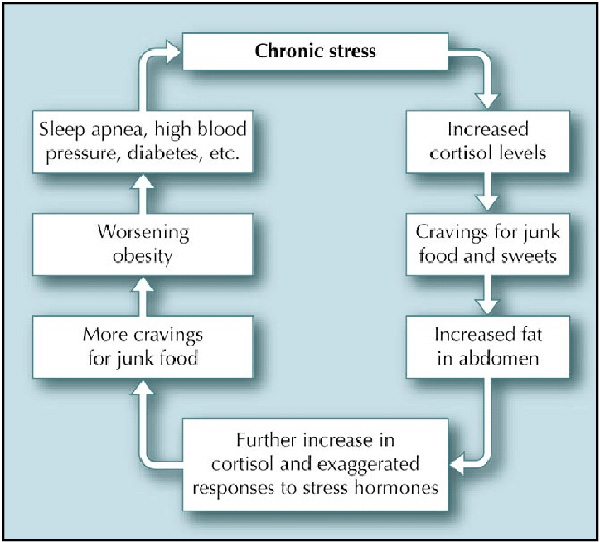
(3)Stress Management: Incorporate stress management techniques
(4) Anti-Obesity medications: Another therapeutic option to manage obesity and the metabolic complications non-surgically, is via anti-obesity medications. These medications are prescribed in addition to the lifestyle changes described above. Anti-obesity medications work via a number of different ways, however in general help with either satiety and/ or satiation. While anti-obesity medication will usually be required on a long-term basis, data on long term safety and effectiveness of such medication is limited.
For example:
Anti-obesity medication may be considered, in individuals who:
- experienced insufficient metabolic health improvements in response to lifestyle modification alone
- in conjunction with a VLED [in many patients results in a greater reduction in adiposity and subsequent metabolic health improvement than if only used one therapy]
- are weaning off VLED
- prior to the removal/elimination of an intragastric balloon
- have experienced a partial response to bariatric metabolic surgery
- have experienced a relapse of their obesity and/or metabolic ill-health after bariatric metabolic surgery
- have experienced a relapse of their obesity and/or metabolic ill-health after any anti-obesity therapeutic intervention
- prior to elective surgery (eg orthopedic, back, abdominal, gynaecological including IVF) to reduce the peri-operative risks
(5) Very Low Energy Diet (VLED): The aim of a VLED is to reduce your energy intake to less than 3300kj/day (800 kcal/day) by substituting meals with formulated meal replacements. It should be noted that VLEDs do not contain pharmacologically-active ingredients. They can be either a protein shake, bar or other. VLEDs can be considered an initial weight loss strategy, when an individual has not responded to supervised lifestyle interventions alone, or when rapid weight loss is required (e.g. prior to bariatric or general surgery conditional on weight loss). While following a VLED, physical activity should be encouraged. VLEDs are low in carbohydrate, inducing a mild ketosis after 2-3 days, which in itself has an anorexic effect.











