Laparoscopic Adjustable Gastric Band (LAGB)
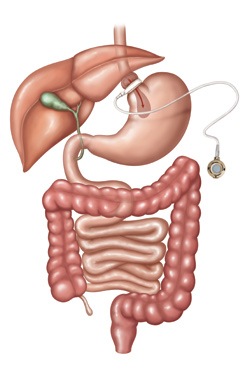
Laparoscopic adjustable gastric banding, commonly referred to as lapbanding, is a minimally invasive weight-loss operation that has been performed in Australia for over 30 years. It essentially involves placing a silicone band around the upper part of the stomach. The LAGB is made of soft silicone and is equipped with a firmly attached inflatable balloon component. This balloon component is connected to an access port via a tube.
The band is positioned around the upper part of the stomach via keyhole (laparoscopic) surgery, so as to create a small pouch. This has a capacity of approximately 15-20ml. The band helps individuals lose weight via two mechanisms:
- By slowing down the rate of food consumption, allowing the stomach adequate time to send feedback to the hunger centre of the brain
- Applying gentle pressure along the axial plexus of nerves which send messages of satiation and satiety to the hunger centre of the brain
The above-mentioned access port is situated under the skin, usually in the upper abdomen area and is easily accessible by the treating doctor via a special needle. By adding/ removing normal saline (sterile water) to the port, it adjusts the volume of fluid in the balloon component of the band, and hence the size of the gastric pouch outlet.
As with any other treatment modality, the lapband is a tool which is part of an overall healthy lifestyle process. The weight loss and health improvements often take approximately 18-24 months to achieve. The science but also clinical experience, tells us that those patients with a LAGB who attend regular follow-up at Clinic experience better health outcomes than those that don’t.
The “gastric band zones” act as a guidance, especially for patients with a LAGB. However, it is up to the treating doctor to determine if adjusting your band is clinically needed or not. It must be noted that if a LAGB is over-tightened, it makes it difficult for an individual to consume healthy nutritious solid food, however slider foods and liquid calories still go down very easily which are not a healthy choices, hence defeating the purpose. This is known as maladaptive eating.
LAGB Indications:
The LAGB may be considered in patients:
With a BMI >40 kg/m2
With a BMI >30 and a complication of obesity or a medical condition associated with obesity
LAGB Contraindications include, but are not limited to:
The LAGB is not permitted in patients who have:
Gastrointestinal or inflammatory disease of the bowel ego esophagitis, ulcers, Chron’s
Severe heart, lung or liver disease
A history of auto-immune diseases such as scleroderma or SLE
Recent history of alcohol or drug dependence
Chronic pancreatitis (inflammation of the pancreas)
Risks associated with lapbanding:
- Vomiting/ regurgitation:
- Some patients have trouble adjusting to the “eating with a band” rules, and so find themselves eating too quickly or too much at any one time, and then regurgitate.
- Repeated regurgitation and/or vomiting can result in band slippage (see below) and a host of other health and nutritional problems. Therefore, patients should contact the Clinic immediately if they are vomiting frequently.
- Leak:
- The gastric balloon component is made of fragile material, and if too much fluid is injected into the lapband, leakage may occur.
- Leakage from the connecting tube can occur if the injecting needle is inserted incorrectly.
- Leakage from the port can occur if the incorrect needle is used for performing an adjustment
- Leakage from the LAGB or from the connecting tube between the balloon component and the port component, may occur.
- It is imperative that an experienced person adjusts your lapband
- If a leak does occur, the gastric band can often be replaced with a new one, however this will require another operation under general anaesthesia.
- Slippage of the band and pouch enlargement
- This occurs in approximately 3% of patients which is much lower than 20 years ago. In recent years the surgical technique has improved significantly, including special measures to secure the band at the time of surgery.
- This problem can arise months, more often years, after the operation.
- It can occur if the “eating with a band” rules are ignored, or due to an overtight band.
- If it does occur, it will require another operation under general anaesthesia.
- Infection of the wound, port and/ or band
- Uncommon, occurring in approximately 1-2% of patients.
- May require treatment with either drainage of the infection, antibiotics and/or removal of the lapband system.
- Band Erosion:
- Uncommon, occurring in approximately 2% of patients; often occurs 3-5+ years after the operation.
- The LAGB may migrate from the outside of the stomach and make its way into the stomach
- More common in patients whose band is over tightened, but it can occur in patients with an appropriate amount of fluid in the LAGB
- If this occurs, it needs to be removed via laparoscopic surgery +/- endoscopy
Suboptimal initial-response to Metabolic Bariatric Surgery [MBS]
i.e. unusually modest improvement in a significant obesity-related health condition
- Partial-responders vs non-responders to treatment
- At present, there is no pre-operative testing that can be done to determine how you will respond to this or any particular therapy
- However, you might be suitable for add-on therapy eg obesity-modifying medication or a variety of other surgical options











