Laparoscopic Gastric Bypass (GBP)
Laparoscopic Roux-en-Y Gastric Bypass (RYGBP)
The laparoscopic Roux-en-Y Gastric Bypass (RYGBP) is one of the most commonly performed bariatric metabolic operations worldwide and has for many years been considered the “gold standard” of bariatric metabolic surgery.
It was first done in the 1960s as open surgery (big cut to the skin of the abdomen), however today it is usually performed via laparoscopic (keyhole) surgery.
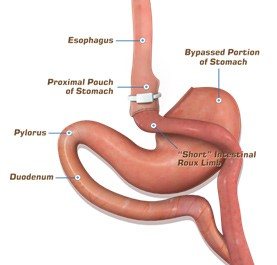
The operation involves sewing and stapling the stomach into two chambers:
- The upper chamber receives food and is very small, with a capacity of approximately 30ml
- The lower stomach chamber is “bypassed” meaning it doesn’t receive food. The small intestine is divided (cut) and one end connected via sewing to the upper stomach chamber pouch (anastomosis=seam=join).
A second connection is sewn (anastomosis=seam) to join the disconnected stomach and duodenum to the small bowel. This connection allows the digestive fluids to mix with the ingested food, thereby allowing nutrient breakdown and absorption by the body.
The distance between the two connections may vary based on surgeon preference, but is usually between 50 to 150cm.
After such an operation, the ingested food travels directly from the small gastric pouch (upper chamber) without passing through the lower portion/chamber of stomach the duodenum and upper small bowel (jejunum). Hence the name “gastric bypass”.
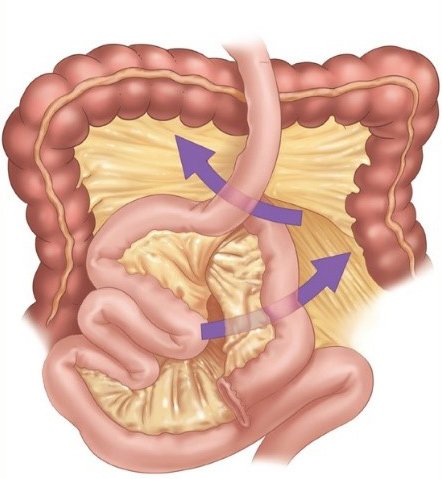
The mesenteric spaces and Petersen’s space (defects in the mesentery) should be closed with non-absorbable sutures to avoid any internal herniation, which could in turn lead to small bowel obstruction. If you develop upper or left sided abdominal pain, please contact our Clinic ASAP- for early intervention as this is a medical emergency! We do NOT want the blood supply to that part of the small intestine to become compromised, as this may result in surgical removal of that part of the small intestine.
There are many postulated mechanisms of action of the RYGBP, including that the small pouch restricts the amount of food that can be consumed at any one sitting.
Secondly, since the food does not go through the bypassed stomach and duodenum, there are metabolic and hormonal changes that lead to reduced appetite and increased feeling of fullness.
The gastric bypass operation reduces the absorption of various micro-nutrients (eg calcium, iron, vitamin B12), which will need to be supplemented and whose levels need to be monitored lifelong. However, it should be noted that this operation does not promote malnutrition. There are other postulated mechanisms of action which can be discussed during your consultation.
Therefore, we recommend having extensive blood tests performed at least once-preferably twice a year, more often if clinically indicated.
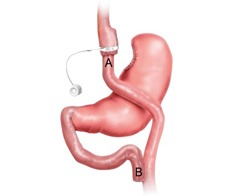
In recent years some surgeons have been placing a silicone ring (Fobi fixed silastic ring) or an adjustable lapband around the small pouch (upper chamber). The science suggests that doing so reduces the risk of hypoglycaemic episodes (sudden drops in blood sugar levels) and also reduces the amount of weight regain at 5 years. However the data to support this in the longer term is still maturing.
Laparoscopic gastric bypass surgery is currently as safe as gallbladder surgery.
At Bariatric Centres which perform a large number of bariatric operations each year, the risk of postoperative complications is low. The risk of dying is less than 0.2%, and the risk of severe complications such as bleeding, infection, clots in legs +/- lungs (DVT +/- PE) is less than 5%.
PE= a DVT which then travels to a lung artery, where it suddenly blocks the blood flow to that part of the lung.
It is more less challenging with the RYGBP compared to the OAGB to access the excluded portion/chamber of stomach for surveillance; this limitation may be an issue in regions with a high incidence of gastric cancer (some Oriental regions).
The gastric bypass appears to have a strong metabolic effect in assisting patients within first 5 years of diagnosis with type 2 diabetes or with pre-diabetes (insulin resistance).
As with any form of therapy, a minority patient who undergo the RYGBP may experience a suboptimal weight loss response (partial- vs non-responders to therapy) and can be offered treatment with either:
- Adjunct obesity-modifying medication OR
- endoscopic interventions OR
- a number of other surgical options.
Laparoscopic One Anastomosis Gastric Bypass (OAGB)
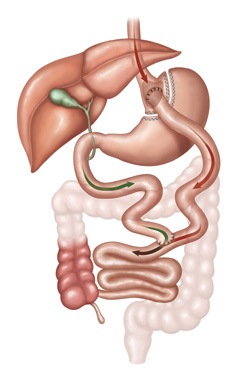
The laparoscopic One Anastomosis Gastric Bypass (OAGB) also known as the omega-loop gastric bypass, was first reported in 2001. During the OAGB operation the surgeon first creates a small “working stomach” which is tube-like in appearance, which is separated by staples and sewing from the rest of the stomach.
This tubular gastric pouch is then sewn and stapled to the intestine, bypassing up to 200cm of the upper part of the intestine. One major difference between this operation and the RYGBP is that this only requires one anastomosis(join) ; the RYGBP required two.
It is believed that the weight loss is achieved via a number of mechanisms which include but are not limited to:
- The newly created smaller gastric tubular pouch can only hold a small quantity if solid food per time
- By bypassing a sizeable segment of the intestine, the remaining intestine is not long enough for normal absorption of nutrients, leading to some malabsorption( especially fats).
Long-term data shows that the OAGB may result in slightly higher weight loss and better resolution of diabetes than the RYGBP. The observed higher diabetes remission rate in OAGB might be attributed to both the greater weight loss and the longer by-passed limb.
The OAGB has few long-term complications, less than 5% of patients require revisional surgery, with half of the revisional operations due to severe malnutrition and the other half due to bile reflux, ulcers or weight regain.
Disadvantages of the OAGB include:
Greater likelihood that patients with OAGB will experience greater bile reflux than after the RYGBP, which will likely require ongoing medication to try and manage it, however can adversely affect one’s quality of life.
Greater likelihood to develop significant vitamins and mineral deficiencies over time, making it critical that patients take their prescribed vitamins and supplements as instructed lifelong, including the fat soluble vitamins A, D, E and K.
Therefore, we recommend having extensive blood tests performed at least once-preferably twice a year, more often if clinically indicated.
The OAGB is more difficult than the RYGBP to access the excluded portion/chamber of stomach for surveillance; this limitation may be an issue in regions with a high incidence of gastric cancer (some Oriental regions).
Some patient who undergo the OAGB may experience a suboptimal weight loss response (partial- vs non-responders to therapy) and can be offered treatment with either:
- Adjunct obesity-modifying medication OR
- endoscopic interventions OR
- a number of other surgical options.